Why there is no quick fix to the threat of avian influenza outbreak
Published on 02/12/2019
CDC/ Erskine. L. Palmer, Ph.D.; M. L. Martin
The search for a broadly protective influenza vaccine – one that could guard against the many strains of the influenza-causing virus – has been in the news recently. The prospect of one influenza vaccine is an exciting one. However, the challenges to making this a reality are great.
Influenza is caused by a virus that is found in many diverse animals, including dogs, bats, seals – and both chickens and people, the focus of our One Health Poultry Hub.
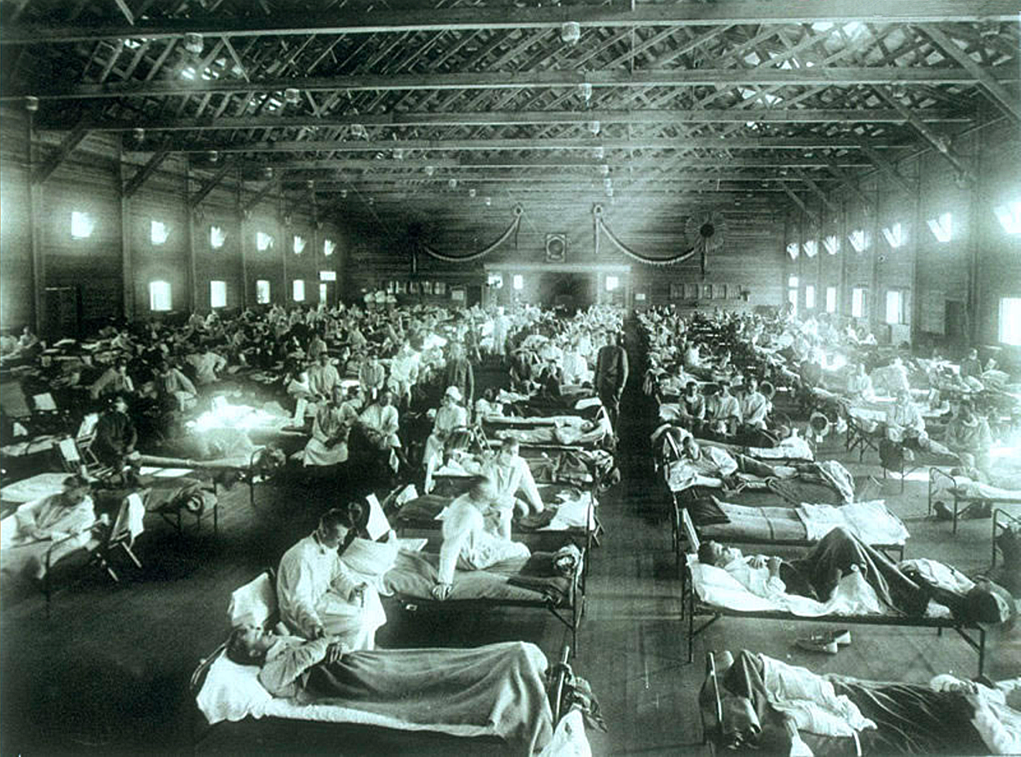
In susceptible animals, such as humans, influenza manifests as a respiratory disease, causing fever, aches, nasal congestion and a cough which together we colloquially refer to as ‘flu’. Though usually influenza is a mild disease like the ‘common cold’, it can kill. The swine flu pandemic of 2009 is estimated to have killed more than 280,000 people and the Spanish flu pandemic of 1918 more than 50 million.
Vaccination strategies
The most effective method of preventing the spread of influenza viruses is with vaccination. Currently, we often vaccinate ourselves against seasonal human strains of the virus (though this has proved more challenging in less-developed countries). We also often vaccinate economically important livestock against host-specific strains; chickens can be vaccinated against endemic avian influenza viruses, while horses can be vaccinated against equine influenza viruses.
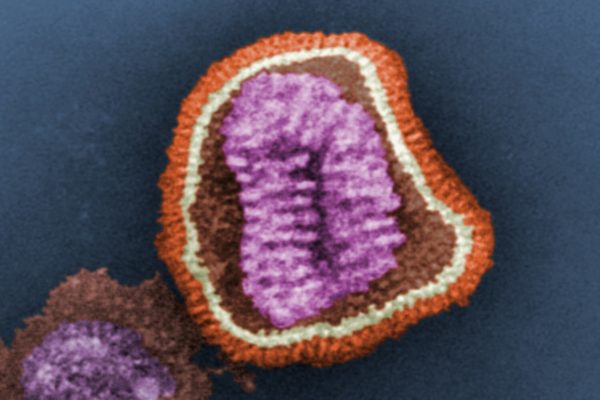
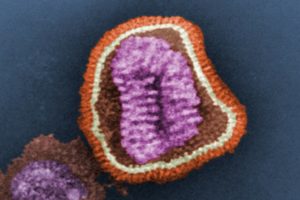
The purpose of most influenza vaccines is to ‘program’ the host’s immune system to combat infection by producing antibodies against proteins found on the surface of the influenza virus which are important for its infectivity. These proteins – haemagglutinin (HA) and neuraminidase (NA) glycoproteins – facilitate the virus’s entry and exit (i.e. infection) of host cells. If neutralised by antibodies, they end the infection.
Virus evolution
However, influenza viruses can mutate and evolve at a rapid rate. Influenza viruses can gain key mutations that help them avoid neutralising antibodies. The result is that frequent, often annual, update of vaccine strains in humans is required to protect against prospective seasonal influenza viruses.
In farmed poultry across northern Africa and the Middle East, and in South and Southeast Asia where our Hub is working, the circulation of avian influenza viruses is continual and high (known as ‘hyperendemic’), leading to the breakdown of vaccine efficacy. The result is substantial economic losses to poultry production systems – and a heightened risk that the avian influenza virus will jump the species barrier to humans. Thus, in order to reduce this risk, prevention and control of avian influenza in poultry is critical.
When a new strain of influenza emerges and infects humans, such as one resulting from viral mutation or evolution – or jumping from another species – existing immunity cannot recognise or deal with it. There is then the risk of a pandemic with dire consequences.
New approaches
To meet the enormous challenge facing influenza vaccination there are several new approaches currently under way. These aim to elicit antibodies against the influenza protein regions which are more ‘conserved’ among distantly as well as closely related influenza viruses. Conserved regions are important for the functioning of the virus and consequently have reduced mutability, making them ideal for a targeted immune response.
This is the basis of research published in the journal Science recently, where the Krammer Laboratory isolated antibodies from a human who had been naturally infected with a human influenza (H3N2) virus. These antibodies targeted a conserved site of the influenza NA protein and were able to protect mice, a model for mammalian species, from diease and the threat of death. What’s more, the identified antibodies could inhibit multiple Influenza A subtypes and Influenza B viruses.
Alternatively, novel approaches aim to elicit broader immune responses by implementing artificial influenza HA proteins that can provoke an immune response to past, present and future potential viruses. This approach utilises ‘computationally optimised broadly reactive antigens’, known as COBRAs, and strives to drive a broad antibody response.
However, in humans and other long-lived animals, multiple exposures to circulating influenza viruses can prime and then boost immune responses. This has an overall positive effect in dealing with influenza infection.
The chicken challenges
In contrast, vaccination in economically important livestock, such as poultry, is met with additional significant challenges. Farmed poultry have comparatively short lives and thus have none or reduced exposure to multiple strains of influenza. They also have a shorter time frame in which they can be vaccinated, including priming and boosting, to appropriate protective levels – and this time frame is further complicated by the presence of maternal antibodies (antibodies passed from the laying hen to her chicks) which can interfere with a desired immune response.
Furthermore, there is always the threat of infection with highly pathogenic avian influenza (HPAI) viruses – those viruses that have mutated to cause considerably high mortality in chickens.
So, in addition to novel vaccination strategies to induce broader and/or universal immune responses, the Avian Influenza Viruses Group led by Professor Munir Iqbal at The Pirbright Institute is currently developing further new vaccines and vaccination strategies for poultry which aim to:
- Induce fast, strong and long-lasting immune responses in poultry from an early age through the targeted delivery of substances that stimulate an animal’s immune response (antigens) directly to those specialist cells of the immune system that can facilitate an adaptive immune response.
- Engineer live poultry-vaccine viruses which can be delivered to chick embryos in eggs so that the birds, once hatched, remain protected throughout their life due to continuous production of protective antigens.
- Provide ‘passive immunity’ to chickens, whereby neutralising antibodies, that have been carefully isolated and characterised in the lab, are being continually produced by the vaccinated chickens to complement the immune system in fighting invading influenza viruses.
These methods aim to provide sterile immunity against a diversity of viruses to chickens in as little time as possible.
One Health
Influenza is a significant One Health concern, and universal vaccines as well as novel methods of vaccination can greatly benefit One Health approaches. It is plausible that a broadly cross-reactive termed as ‘universal vaccine’ developed for humans could be adapted to be effective in livestock, such as chickens.
Thus, people and livestock could be protected against, respectively, seasonal and enzootic (regularly affecting animals in a particular district or at a particular season) influenza viruses, and people further protected from pandemics that often emerge from livestock. However, the added challenges in chickens would need to be met by expediting the effects of a universal vaccine.
The One Health Poultry Hub is undertaking research to design and develop highly cross-protective and cost-effective vaccines against avian influenza viruses affecting poultry. The availability of such vaccines will be a step-change in reducing ever-increasing threats from these viruses, benefiting animal welfare, public health, economy and the environment globally.