Preventing a future pandemic by imitating natural selection
Published on 04/09/2020

Incessant Flux via Flickr CC BY 2.0
A new type of avian influenza that can infect poultry and humans, called H7N9, emerged in China in February 2013. Since then, there have been over 1,500 confirmed human infections with an estimated 40% case fatality rate.
In the wake of COVID-19, these numbers may seem to be relatively small. But these statistics provide an example of the issues we face in controlling influenza viruses in animals and how understanding more about these viruses can help us to predict, prevent and control outbreaks, protecting both poultry and human health.
Influenza viruses infect a huge range of animals, but the strains that are of greatest concern to us are those that circulate in livestock such as pigs and poultry, where people in farming industries have close contact with the animals. Influenza viruses can rapidly mutate, allowing them to escape the immune responses of the animals they infect and even jump to new species.
There have been five major epidemic waves of H7N9 in China. The final wave in 2016-2017 saw the originally mild disease of poultry mutate to cause higher levels of mortality in chickens and spread almost everywhere in China. The severity of H7N9 avian influenza virus (AIV) situation prompted the Chinese government to implement a mass vaccination programme against H7N9 in poultry in 2017.
Since its use, the number of poultry outbreaks along with human infections has dropped dramatically, with only three human infection cases reported during 2017 to 2018 and one human infection case reported during 2018 to 2019. This may sound like vaccination has solved the problem and the virus will now be eradicated. Unfortunately, this is not the case – despite the reduction in disease outbreaks due to vaccination, these viruses have not been eradicated.
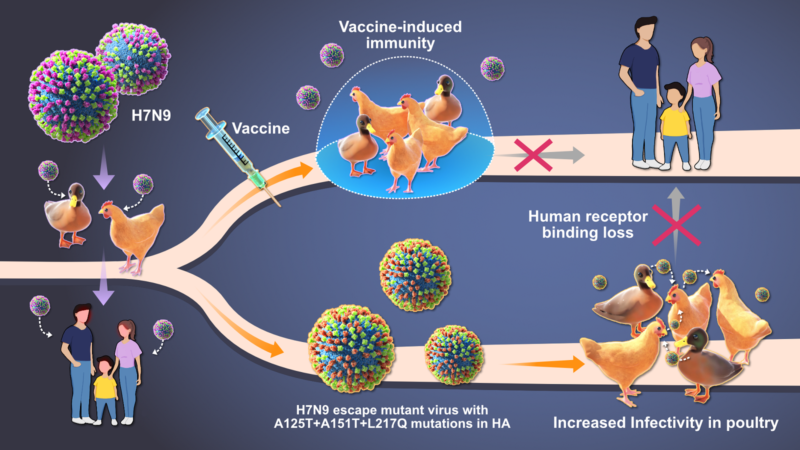
This is partly because of influenza’s high mutation rate – vaccination can inadvertently encourage the evolution of viruses with mutations that allow them to escape vaccine-induced immunity. Once a virus escapes, it can spread rapidly, thereby making the vaccine ineffective and a new one must be designed. This is where our research comes in.
Vaccine-induced mutation
Our aim is to understand how H7N9 viruses could potentially mutate in the field in response to vaccination, and how these genetic changes could alter how the virus acts (for example, by making it more dangerous to poultry or by helping it to infect humans more effectively).
By imitating the natural selection process in the lab, we found several mutations and identified that one specific mutation allows the virus to escape from vaccine-induced immunity. Importantly, three other mutations that we observed in our lab studies had been found in the field in 2019 indicating that our method can predict the evolution of influenza viruses.
These three mutations prevent H7N9 viruses from binding to human cells, but increase their binding, replication and stability in chicken cells and embryos. This could mean that the strains which have these mutations pose a lower threat to human health, but increase the risk to poultry.
Monitoring threats
This shows that mass vaccination of poultry against H7N9 strains in China drives virus evolution away from human pandemic. But viruses with ‘escape mutations’ remain a significant risk to poultry due to their ability to escape vaccine-induced immunity and persist in poultry.
Our studies may also help to explain the Chinese government’s successful control of H7N9 infection in humans by mass poultry vaccination. On one hand, the mass poultry vaccination protects the poultry from H7N9 infection and greatly reduces the risk of human infections as the majority of human H7N9 cases are linked to exposure to infected poultry or contaminated environments. On the other hand, even when some viruses escape the vaccine-induced immunity, they pose reduced risk to humans due to the lost human receptor binding.
However, this may not be the case for all strains. Other mutations may arise in the future that have human pandemic potential or are even more deadly to poultry. Using a method that can predict how vaccination may change influenza virus characteristics is hugely valuable as it can provide advanced warning of mutations that could increase likelihood of human infection. Incorporating these mutations into global health surveillance efforts can help relevant authorities to monitor potential threats and get ahead of them before they have a chance to spiral out of control.
This post originally appeared as a blog on the Newton Fund website.